Project Description
Author: Khan et al.
Summary:
Knowledge and belief about antibiotic use are important modifiers of antibiotic-associated health practices and, thereby, its resistance. Rural people’s knowledge and belief about antibiotic use and their determinants largely remained unexplored in Bangladesh. Hence, this study was aimed.
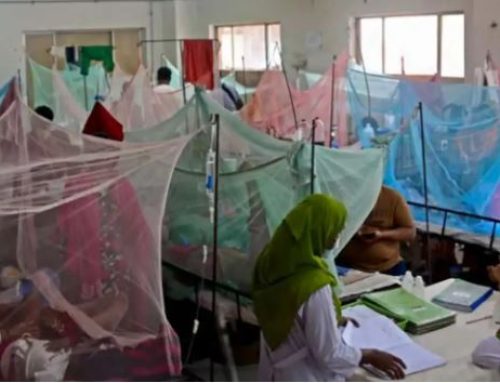
This descriptive cross-sectional study was conducted between July 2016 to March 2017 in Upazila Health Complex, Matlab South, Chandpur, Bangladesh. Adult (≥18 years) residents of the study area coming for health service were approached and a total of 184 participants were selected using a systematic random sampling method. Data were collected by face-to-face interview using a pre-tested structured questionnaire including questions on knowledge and belief regarding antibiotic use. Informed verbal consent was taken before inclusion. The principles laid out by World Medical Association Declaration of Helsinki were following during all the procedures of this study. Data analysis was done in STATA© Version 16.
The average age of the participants was 37.45±13.32 years (SD) with a female predominance (61.4%). Of all, 63% knew about antibiotics, and out of them 59.5% self-prescribed the drug. Among participants who knew about antibiotics 63.9% (n=73) had good knowledge and 47.8% had appropriate belief. On multivariable logistic regression, higher education (SSC and above) (OR 4.67, 95%CI 1.02 – 21.38) and use of the internet and social media (OR 8.27, 95%CI 1.51-45.33) were found to be significant predictors of good knowledge regarding antibiotic use. Moreover, belief regarding antibiotic use showed a significant positive linear association with knowledge (Spearman’s rho=0.4797, p<0.001).
Conclusion: The study found that nearly one-third of rural people had poor knowledge and more than half had inappropriate belief about antibiotic use among rural people in Bangladesh. Authorities and policymakers should urgently address the situation to resist the threat of widespread antibiotic resistance.
Keywords: Antibiotics, Knowledge, Belief, Rural, Resistance, Inappropriate use
Status: Ongoing
Full text link: Not available