Project Description
Author: Paul et al.
Summary:
Introduction: As a mode of delivery, the caesarean section (CS) is a life-saving measure for many cases, but it also may result in short- and long-term hazardous consequences, and scar dehiscence is one of them. Identification of the patients prone to scar dehiscence followed by predictive measures could reduce the associated morbidity and mortality. Scar tenderness was discussed as a predictive sign of scar dehiscence but still, there is a lack of enough evidence. This study aimed to observe the frequency of scar dehiscence among patients undergoing CS presenting with scar tenderness.
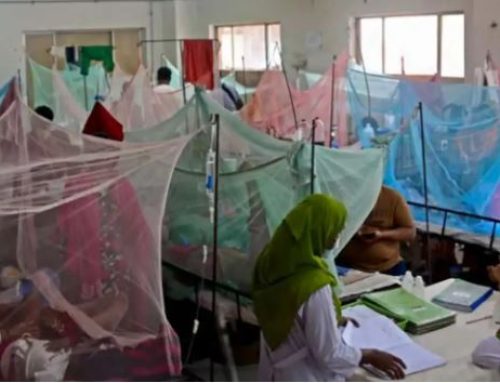
This study was an observational study and was conducted in the Department of Gynecology and Obstetrics, Dhaka Medical College Hospital (DMCH), from January 2018 to June 2018. A total of 50 full-term pregnant women selected for lower segment CS (LSCS), presenting with scar tenderness from previous CS were enrolled. A semi-structured questionnaire was used during data collection. Statistical analyses were done with SPSS V-25.0. All ethical measures were done in accordance with the current Declaration of Helsinki.
The average age of the studied mothers was 28 years. Per-operatively, scar complications were found in 46% of the cases (26% scar thinning, 16% scar dehiscence, and 4% scar rupture). A short inter-delivery interval and a less equipped center as a previous location of CS were associated with scar complications (p<.05). Postoperative maternal complications were observed in 12% of the patients which were, including wound infections, blood transfusion reactions and psychiatric disturbances. The frequency of IUD (intrauterine death) was 2%, and 10% of the neonates needed NICU (neonatal intensive care unit) admission.
Conclusion: about one sixth of the scar tenderness patients had scar dehiscence with considerable amount of other complications. Extensive evaluation before any procedures are therefore suggested for all patients.
Status: Ongoing
Full text link: Not available